 |
 |
 |
 |
 |
 |
What Is Seasonal Affective
Disorder?
A form of depression that follows a seasonal pattern, seasonal
affective disorder (SAD) appears at the same time each year and
disappears at the same time each year. With SAD, a person typically
experiences symptoms of depression as winter approaches and daylight
hours become shorter. When spring returns and the days become
longer again, a person with SAD experiences relief from their
symptoms, returning to a normal mood and energy level.
What Are the Symptoms of
SAD?
Like other forms of depression, the symptoms of SAD can be mild,
severe, or anywhere in between. Milder symptoms interfere less
with someone's ability to participate in everyday activities,
but more severe symptoms can interfere much more.
The symptoms of SAD are the same as those of depression, but simply occur during a specific time of year. It's the seasonal pattern of SAD - the fact that symptoms occur only for a few months each winter (for at least 2 years in a row) but not during other seasons - that distinguishes SAD from other forms of depression.
Symptoms of SAD may include:
* Changes in mood - sadness, irritability, and/or feelings of
hopelessness or worthlessness most of the time for at least 2
weeks; tendency to be more self-critical and more sensitive than
usual to criticism; crying or getting upset more often or more
easily
* Lack of enjoyment - loss of interest in things that are normally
enjoyable; feeling like tasks can't be accomplished as well as
before; feelings of dissatisfaction or guilt
* Low energy - unusual tiredness or unexplained fatigue
* Changes in sleep - sleeping much more than usual (which can
make it difficult for children with SAD to get up and get ready
for school in the morning)
* Changes in eating - craving simple carbohydrates (i.e., comfort
foods and sugary foods); tendency to overeat (which could result
in weight gain during the winter months)
* Difficulty concentrating - more trouble than usual completing
assignments on time; lack of usual motivation (which can affect
school performance and grades)
* Less time socializing - spending less time with friends, in
social activities, or in extracurricular activities
The problems caused by SAD, such as lower-than-usual grades or less energy for socializing with friends, can affect self-esteem and leave people feeling disappointed, isolated, and lonely - especially if they don't realize what's causing the changes in energy, mood, and motivation.
What Causes SAD?
It's believed that with SAD, depression is somehow triggered by
the brain's response to decreased daylight exposure. How and why
this happens isn't yet fully understood. Current theories about
what causes SAD focus on the role of sunlight in the brain's production
of certain key hormones that help regulate sleep-wake cycles,
energy, and mood. Two naturally occurring chemicals in the body,
melatonin and serotonin, are currently thought to be involved
in SAD.
Melatonin, which is linked to sleep, is produced in greater quantities when it's dark or when days are shorter. Increased production of melatonin can cause sleepiness and lethargy. Serotonin production increases with exposure to sunlight. Low levels of serotonin are associated with depression, so increasing the availability of serotonin helps to combat depression. Shorter days and longer hours of darkness in fall and winter may cause increased levels of melatonin and decreased levels of serotonin, the combination of which may create the biological conditions for depression.
How Is SAD Treated?
Treatment for SAD, which varies depending on the severity of the
symptoms, includes:
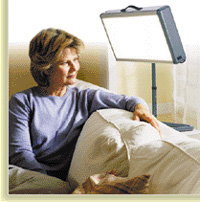
Increased Light Exposure - Because the symptoms of SAD are triggered
by lack of exposure to light and tend to go away on their own
when available light increases, treatment for SAD often involves
increased exposure to light during winter months. For someone
with mild symptoms, it may be enough to spend more time outside
during the daylight hours, perhaps by exercising outdoors or taking
a daily walk. Full spectrum (daylight) lightbulbs that fit in
regular lamps can help bring a bit more daylight into your home
in winter months and might help with mild symptoms.
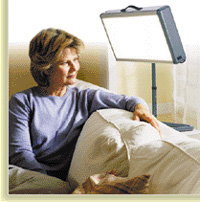
Light Therapy (or phototherapy) - Stronger symptoms may be treated with light therapy involving the use of a special stronger light that simulates daylight. A special light box or panel is placed on a tabletop or desk, and the person sits in front of the light for a short period of time every day (45 minutes a day or so, usually in the morning) with their eyes open, glancing - not staring - occasionally at the light (to work, the light has to be absorbed through the retinas). Symptoms tend to improve within a few days in some cases or within a few weeks in others. Generally, light therapy is used until enough sunlight is available outdoors. Some mild side effects of phototherapy might include headache or eyestrain.
Lights that are used for SAD phototherapy must filter out harmful UV rays. Tanning beds or booths should not be used to alleviate symptoms of SAD. The ultraviolet rays emitted by tanning beds can damage skin and cause wrinkles, age spots, and even lead to skin cancer such as melanoma. Phototherapy should be used with caution if your child has: another type of depressive disorder, skin that's sensitive to light, or medical conditions that may make his or her eyes vulnerable to light damage. Be sure to discuss any of these situations with your child's doctor. Like any treatment, phototherapy should be used under the supervision of your child's doctor.
Medication (or pharmacotherapy) - Medications, which might be used in combination with talk therapy and light therapy, may be prescribed for a child or a teen with SAD and should be monitored by a doctor. Antidepressant medications help to regulate the balance of serotonin and other neurotransmitters in the brain that affect mood and energy. Be sure to let your child's doctor know about any other medications he or she may be taking, including over-the-counter or herbal medicines, which could interfere with prescription medications.
Talk Therapy (or psychotherapy) - Helping to ease the sense of isolation or loneliness, talk therapy focuses on revising the negative thoughts and feelings associated with depression. Talk therapy can also help people with SAD to learn about and understand their condition as well as learn what to do to prevent or minimize future bouts of seasonal depression.
What Parents Can Do?
If you suspect your son or daughter has SAD, talk to your child's
doctor about your concerns. Doctors and mental health professionals
make a diagnosis of SAD after a careful evaluation. A medical
checkup is also important r to make sure that symptoms aren't
due to a medical condition that needs treatment. Tiredness, fatigue,
and low energy could be signs of another medical condition such
as hypothyroidism, hypoglycemia, or mononucleosis. Other medical
conditions can cause extreme fatigue or changes in appetite and
sleep.
When symptoms of SAD first develop, a parent may mistakenly think that his or her child is slacking off or not trying. It's not uncommon for parents to attribute low motivation, energy, and interest to an intentional poor attitude. Learning about SAD can help parents understand another possible reason for the changes, easing feelings of blame or impatience with their child or teen.
Parents are sometimes unsure of how to discuss their concerns and observations with their child or teen. The best approach is usually one that's supportive and non-judgmental. Opening the discussion (using your own words) in the following way may be helpful: "You haven't seemed yourself lately - you've been so sad and grouchy and tired, and you don't seem to be having much fun. It seems like you've been feeling kind of worn out and exhausted - like you just can't get enough sleep. So, I've made an appointment for you to get a checkup. I want to help you to feel better and get back to doing your best and enjoying yourself again."
Here are a few things you
can do if your child or teen has been diagnosed with SAD:
* Participate in your child's treatment. Ask the doctor how you
can best help your child.
* Help your child understand SAD. Learn about the disorder and
provide simple explanations. Remember, concentration might be
difficult, so it's unlikely your child will want to read or study
much about SAD - recap the main points for him or her if symptoms
are strong.
* Encourage your child to get plenty of exercise and to spend
time outdoors. Take a daily walk together.
* Find quality time. Spend a little extra time with your child
- nothing special, just something low key that doesn't require
much energy. Bring home a movie you might enjoy or share a snack
together. Your company and caring is the key ingredient. It's
helpful to provide personal contact and a sense of connection.
* Be patient. Don't expect symptoms to go away immediately. Remember
that low motivation, low energy, and low mood are part of SAD
- it's unlikely that your child will respond cheerfully to your
efforts to help.
* Help with homework. You may have to temporarily provide hands-on
assistance to help your child organize assignments or support
your child in completing work. Let your child know that concentration
problems are part of SAD and that things will get better again.
Kids and teens with SAD may not realize this and may worry that
they aren't capable of doing the schoolwork. You may also want
to talk to your child's teacher - ask for extensions on assignments
until things get better with treatment.
* Help your child to eat right. Encourage your child to avoid
loading up on simple carbohydrates and sugary snacks. Provide
plenty of whole grains, vegetables, and fruits.
* Establish a sleep routine. Encourage your child to stick to
a regular bedtime every day so they can reap the mental health
benefits of daytime light.
* Take it seriously. Don't put off evaluation if you suspect you
child may be experiencing depression. If your child has SAD, help
your child learn about the seasonal pattern of his or her depression.
Talk with your child - and let your child talk about what he or
she is experiencing. Reassure your child that things will get
better, even though that may seem impossible right now.
Disclaimer: This information is not intended be a substitute for professional medical advice. It is provided for educational purposes only. You assume full responsibility for how you choose to use this information.
Reviewed by: Stephen Lee Cosby,
MD
Date reviewed: January 2004